Linda Millband is the national practice lead for medical negligence at Thompsons Solicitors.
She led the team responsible for fighting, and winning, a legal battle on behalf of 650 ex-patients of disgraced breast surgeon Ian Paterson. With the Independent Inquiry into Ian Paterson’s report due in a matter of days, Linda reflects on how it should be used as a catalyst for positive change in private hospitals.
Ian Paterson: the story so far
No one knows why Ian Paterson carried out hundreds of unnecessary operations on people who didn’t need them, because he has refused to say. What we can say with certainty is that he benefitted financially from doing so.
Ian Paterson has been in jail since 2017. He is now three years into a 20-year sentence for multiple counts of wounding with intent. But, for the 650 individuals who turned to Thompsons to represent them in the wake of one of the worst health scandals in recent times, justice will not be done until the root cause of what went so wrong, and how he was allowed to carry on for so long, is laid bare.
On 4 February 2020 our clients may start to get some answers when the Lord Bishop of Norwich publishes the findings of his independent Inquiry.
The spotlight must be on private healthcare
Ian Paterson didn’t abuse a system; rather he took every advantage available to him while working within it. The structure of the private hospitals where he worked allowed him to hide negligent, criminal actions for years – giving hundreds of people operations they didn’t need, handing down cancer diagnoses to people who did not have the disease, and removing breasts and other organs that did not need to be removed.
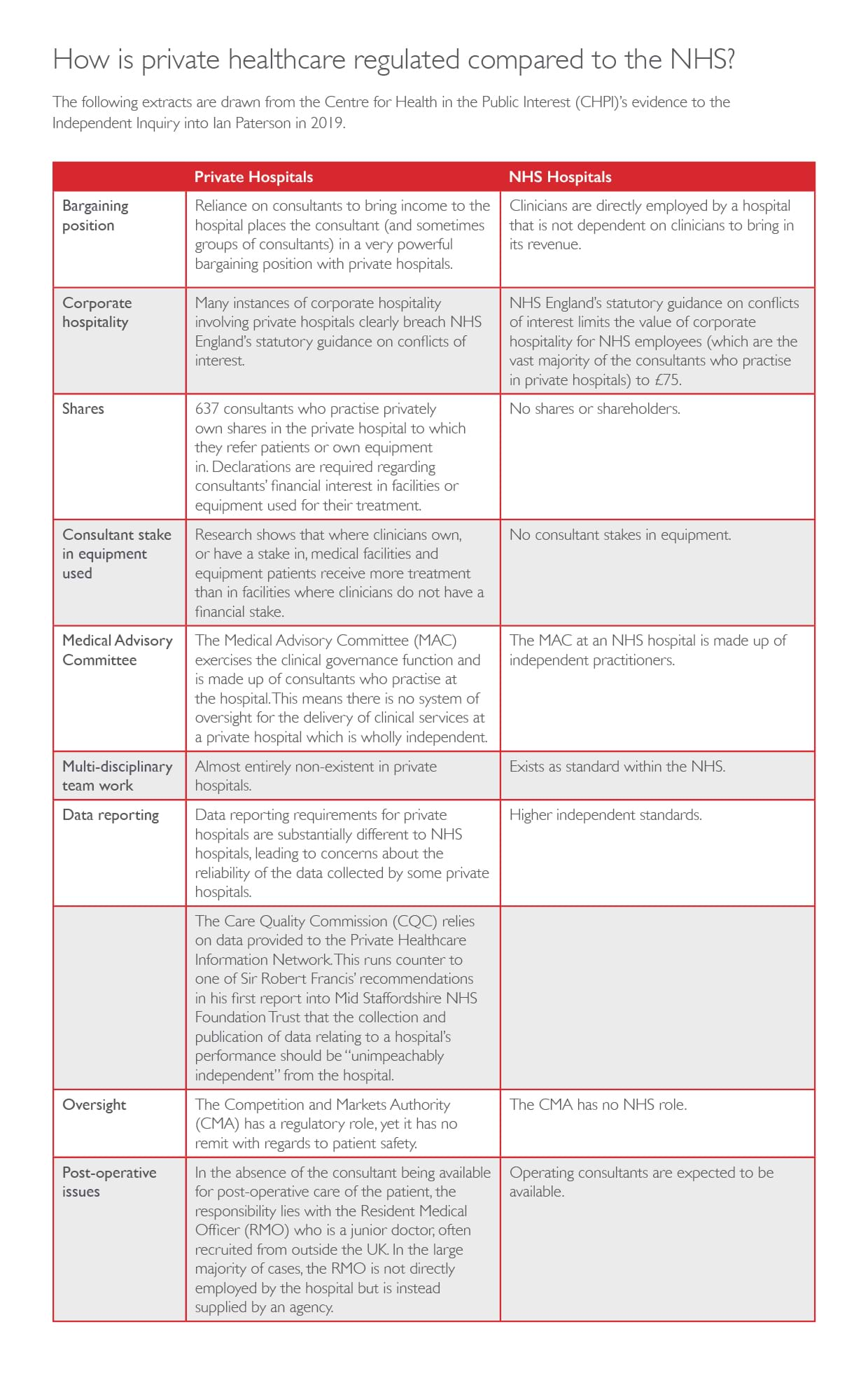
Abuse on this scale, and of this magnitude, lays bare one of many fundamental flaws in the UK’s private healthcare system. Private hospitals and the surgeons they contract with (note, ‘contract’ not ‘employ’) get to ‘play God’ - making decisions about what, and how many, surgical procedures a patient may need whilst ‘marking their own homework’ in a way that is unthinkable in the NHS. Private hospital Medical Advisory Committees - who are meant to provide oversight - are made up of consultants who practice at those hospitals. And they are able to line their pockets in the process.
Putting profits before patients
With money getting in the way of care, we are seeing more and more patient recalls after unnecessary surgery at private hospitals.
While he is probably one of the most notorious examples, Ian Paterson is not a ‘lone wolf’. He is just one example of why the private healthcare sector is in need of urgent reform to make sure patient safety is no longer compromised by the pursuit of profit.
What went wrong at Spire Healthcare?
Paterson was able to take advantage of a series of ‘grey areas’ in order to slip between the cracks while working at Spire Healthcare. Without robust multi-disciplinary team (MDT) structures – like those used by the NHS to ensure no one clinician has total power of a patient’s treatment plan – Paterson was able to make stand-alone decisions about surgeries patients did, or didn’t need, and then charge them for the privilege.
Private hospitals passing the buck
For its part, Spire Healthcare tried to ‘look the other way’ on Paterson (and it is continuing to do so in other patient recalls since for surgeons operating at its hospitals). This is because it employs a business model designed, according to Centre for Health and the Public Interest, to ‘insulate [them] from the liability and costs of having to compensate patients who are harmed and injured’. The ‘why’ maybe financially self-evident but the ‘how’ isn’t well-known or appreciated
Many consultants at private hospitals are NHS doctors working freelance. According to the private providers, the lack of an employment relationship makes regulating consultants the NHS’ problem, and when things go wrong they can deny responsibility saying (as one nurse told one of our Paterson clients) that they ‘only rented him a room’.
Add to the mix that 637 consultants who practise in private hospitals own shares in private healthcare and some own, or have a stake in, the equipment they use there and it’s a very different world from their day jobs in the NHS. And given that private hospitals with critical care facilities (sometimes known as intensive care units) are rare, if something goes seriously wrong a private hospital patient is usually transferred to a local NHS hospital for them to pick up the pieces (at no cost to the private hospital who made the mistakes).
What does this mean for patients?
This means that a private hospital group like Spire can sell you a service or treatment, put you in touch with a consultant, charge you for the treatment, provide that treatment at its hospital by a consultant (working on their own) who may have shares in the company and/or be using equipment they own, and yet dump you back on the NHS and leave you out in the cold, and without compensation, if something goes wrong.
It’s a dangerous ‘liability loophole’ that puts patients at significant risk if they choose private treatment, that just does not exist for NHS patients. By comparison, the NHS – while not immune from instances of negligence – has systems and structures set up to minimise instances of patient harm, and processes for how it deals with it when things go wrong on its watch. Our experience is that they ‘put their hands up’ when things go wrong, whereas private hospitals dig in.
What needs to be changed to protect patients?
The ‘liability loophole’ can be closed by making sure consultants who operate at private hospitals are directly employed by those hospitals, introducing MDTs, proper oversight and transparency on ownership. This will ensure that – for the first time – private hospitals have to start regulating consultants’ actions, not just count the profits generated by those actions. The forthcoming Inquiry’s report can be game-changing – and give those for whom we acted, who were butchered by an unchecked monster – a sense of hope for real change.
Thompsons Solicitors has been campaigning to improve patient safety within private healthcare following its central role in representing 650 of Ian Paterson’s victims.